Do you know what BMAC injecton is?
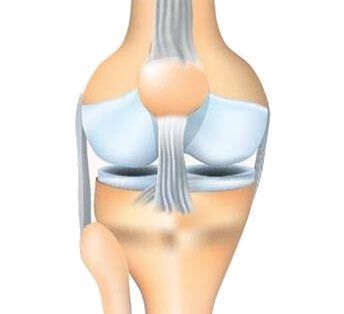
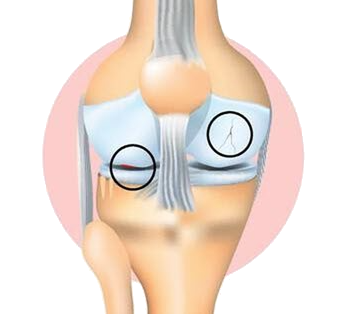
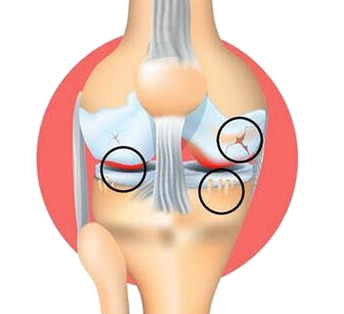
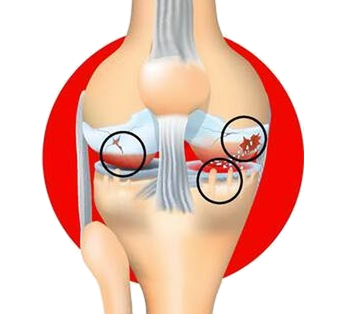
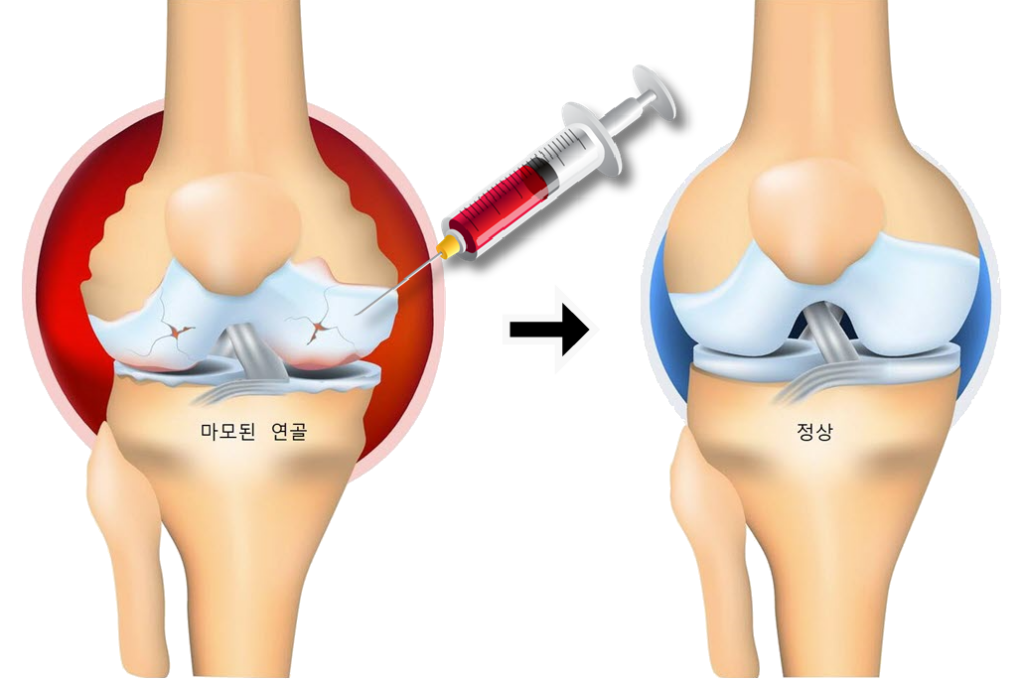
When you're young, your knee joint is healthy, but as you age, the cartilage and surrounding tissue wears away, causing inflammation, swelling, and pain. Cartilage has no blood vessels and no stem cells to regenerate it, so once it's damaged, it can't regenerate itself.
As degenerative arthritis progresses, the last resort is "joint replacement surgery". This is when autologous bone marrow aspirate concentrate injections become an alternative.
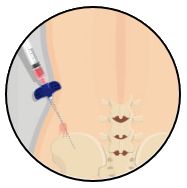
Centrifuging bone marrow taken from the patient's hip and injecting it into the knee joint as a bone marrow aspirate concentrate (BMAC) can help relieve pain and improve function.
- 1It uses autologous bone marrow, so there is no immune rejection.
- 2The autologous bone marrow harvest is performed under local anesthesia, making the process simple.
- 3
They are not cultured externally, so there is no risk of genetic modification.
- 4
It's a quick procedure, and it's not just a temporary fix.
Procedure for Autologous Bone Marrow Aspirate Concentrate
To accurately diagnose a patient's knee joint condition, imaging modalities such as MRI or X-ray will be used to assess the extent of cartilage damage and progression of degenerative arthritis to determine if an autologous bone marrow aspirate concentrate injection may be effective.
Who should receive BMAC injections
Patients with degenerative arthritis who have cartilage damage but no leg bone deformity may benefit from treatment. In the late stages of degenerative arthritis, when the cartilage in the knee has completely worn away, treatment with autologous bone marrow is not very effective, and artificial joint surgery should be considered.
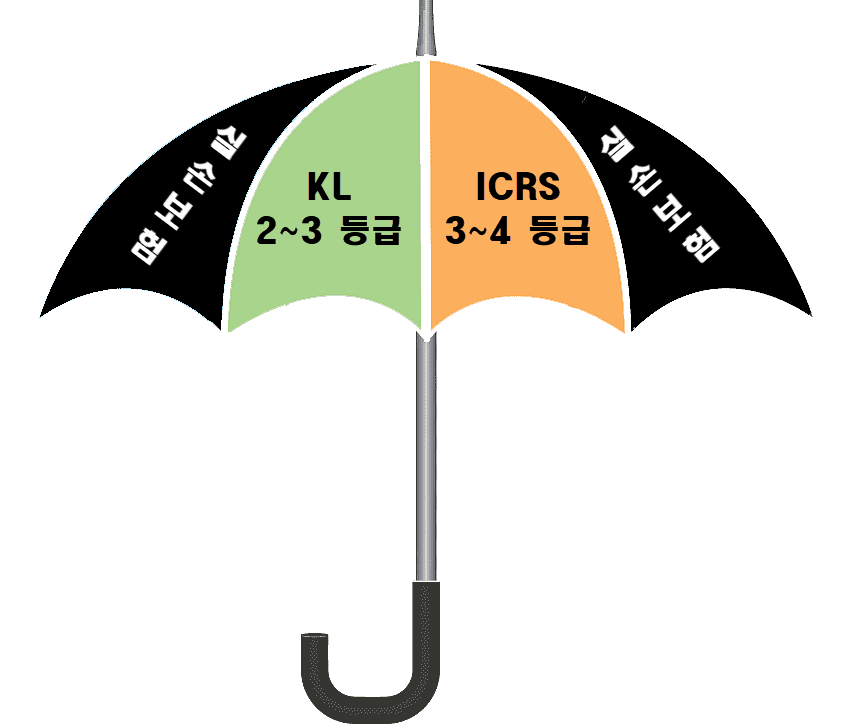
There are two grades for imaging: KL, which indicates the degree of degenerative arthritis, and ICRS, which indicates the degree of cartilage damage. KL Grade 2-3and ICRS grade 3~4with knee osteoarthritis is a candidate for a BMAC injection.
👉 Patients with grade 1 arthritis with less severe symptoms or grade 4 arthritis with more advanced arthritis may not see much benefit.
Autologous Bone Marrow Aspirate Concentrate Injection Loss and Damage Insurance
Autologous bone marrow treatment for knee osteoarthritis was recognized as a "new medical technology" by the Ministry of Health and Welfare in July 2023, which means that the safety and efficacy of the treatment has been legally proven, and therefore it can be covered by accidental death and dismemberment insurance.
And based on the grade of your X-ray, MRI, or arthroscopy, you must meet the following requirements to be eligible for loss of income coverage
① The joints have a clear narrowing of the gap (KL grade 2-3)
② Patients with arthritis with cartilage damage of 50% or greater (ICRS grade 3-4).
| Traditional treatments | Autologous Bone Marrow Aspirate Concentrate Injection |
|---|---|
| Applied through a small incision Requires anesthesia Weight-bearing restrictions for 3 to 6 weeks after surgery Cartilage defect area 2 to 9 cm2 The cost of treatment is around 10 million won |
Injections without incisions No anesthesia required Resume normal activities immediately after treatment Cartilage defect area is not limited 1/3 the cost of traditional care |